Do Fallen Arches Require Surgery?
Overview

Flat feet (also called pes planus or fallen arches) is a postural deformity in which the arch of the foot collapses, with the entire sole of the foot coming into complete or near-complete contact with the ground. Some individuals (an estimated 20-30% of the general population) have an arch that simply never develops in one foot (unilaterally) or both feet (bilaterally).
Causes
Flat feet in adults can appear for a number of reasons. Arches never developed properly. Damage to the tendons that support the arch. Damage or inflammation of the posterior tibial tendon which runs from your lower leg, down and across your ankle, and connects to the middle of the arch. Trauma involving broken bones in the foot. Rheumatoid arthritis. Aging, pregnancy, nerve damage, obesity or even diabetes.
Symptoms
The majority of children and adults with flexible flatfeet never have symptoms. However, their toes may tend to point outward as they walk, a condition called out-toeing. A person who develops symptoms usually complains of tired, aching feet, especially after prolonged standing or walking. Symptoms of rigid flatfoot vary depending on the cause of the foot problem. Congenital vertical talus. The foot of a newborn with congenital vertical talus typically has a convex rocker-bottom shape. This is sometimes combined with an actual fold in the middle of the foot. The rare person who is diagnosed at an older age often has a "peg-leg" gait, poor balance and heavy calluses on the soles where the arch would normally be. If a child with congenital vertical talus has a genetic disorder, additional symptoms often are seen in other parts of the body. Tarsal coalition. Many people have no symptoms, and the condition is discovered only by chance when an X-ray of the foot is obtained for some other problem. When symptoms occur, there is usually foot pain that begins at the outside rear of the foot. The pain tends to spread upward to the outer ankle and to the outside portion of the lower leg. Symptoms usually start during a child's teenage years and are aggravated by playing sports or walking on uneven ground. In some cases, the condition is discovered when a child is evaluated for unusually frequent ankle sprains. Lateral subtalar dislocation. Because this often is caused by a traumatic, high-impact injury, the foot may be significantly swollen and deformed. There also may be an open wound with bruising and bleeding.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
pes planus orthotics
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment

Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
Prevention
Sit up straight in a chair with your feet flat on the ground. Scrunch up the toes of one foot as if you are trying to grab hold of the floor then use your toes to drag your foot a small distance forwards. Do this a couple of times on each foot, but don?t use your leg muscles to push your foot forward -- the movement should come solely from the muscles in your feet. Sit in a chair and place a cleaning cloth, towel or small ball on the floor at your feet. Use the toes of one foot to grasp the object and lift it off the floor. This action will require you to clench your toes and contract your arch. Once you have lifted the object a little way off the floor, try to throw it in the air and catch it by stretching your toes and arch out and upwards. Repeat the exercise several times on both feet. Sit on the floor with your legs straight out in front of you then bend your knees out to either side and place the soles of your feet together so your legs form a diamond. Hold on to your ankles and, keeping your heels together at all times, separate your feet so your toes point out to either side. Open and close your feet in this way several times, making sure your little toes stay in contact with the floor throughout the exercise. Starting in the same position, try separating your heels, keeping your toes together at all times.

Flat feet (also called pes planus or fallen arches) is a postural deformity in which the arch of the foot collapses, with the entire sole of the foot coming into complete or near-complete contact with the ground. Some individuals (an estimated 20-30% of the general population) have an arch that simply never develops in one foot (unilaterally) or both feet (bilaterally).
Causes
Flat feet in adults can appear for a number of reasons. Arches never developed properly. Damage to the tendons that support the arch. Damage or inflammation of the posterior tibial tendon which runs from your lower leg, down and across your ankle, and connects to the middle of the arch. Trauma involving broken bones in the foot. Rheumatoid arthritis. Aging, pregnancy, nerve damage, obesity or even diabetes.
Symptoms
The majority of children and adults with flexible flatfeet never have symptoms. However, their toes may tend to point outward as they walk, a condition called out-toeing. A person who develops symptoms usually complains of tired, aching feet, especially after prolonged standing or walking. Symptoms of rigid flatfoot vary depending on the cause of the foot problem. Congenital vertical talus. The foot of a newborn with congenital vertical talus typically has a convex rocker-bottom shape. This is sometimes combined with an actual fold in the middle of the foot. The rare person who is diagnosed at an older age often has a "peg-leg" gait, poor balance and heavy calluses on the soles where the arch would normally be. If a child with congenital vertical talus has a genetic disorder, additional symptoms often are seen in other parts of the body. Tarsal coalition. Many people have no symptoms, and the condition is discovered only by chance when an X-ray of the foot is obtained for some other problem. When symptoms occur, there is usually foot pain that begins at the outside rear of the foot. The pain tends to spread upward to the outer ankle and to the outside portion of the lower leg. Symptoms usually start during a child's teenage years and are aggravated by playing sports or walking on uneven ground. In some cases, the condition is discovered when a child is evaluated for unusually frequent ankle sprains. Lateral subtalar dislocation. Because this often is caused by a traumatic, high-impact injury, the foot may be significantly swollen and deformed. There also may be an open wound with bruising and bleeding.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
pes planus orthotics
Non Surgical Treatment
Treatment isn't usually needed for flat feet because the condition doesn't usually cause any significant problems. Aching feet can often be relieved by wearing supportive shoes that fit properly. You may need to wear shoes that are wider than normal. If your feet overpronate, you may need to wear a special insole (an orthotic) inside your shoes to stop your feet rolling inwards when you walk or run. These will usually need to be made and fitted by a podiatrist. Stretching your calf and Achilles tendon may also help as a tight Achilles can make your foot overpronate. To stretch your calf and Achilles tendon, step forwards with your left leg and bend it, with your right leg straight and both feet pointing forwards, push your right heel into the ground while keeping your right leg straight; you should feel the stretch at the back of your right leg, below the knee, hold the stretch for 15 to 30 seconds and repeat with the opposite leg, repeat the stretch two to four times on each leg, and repeat the overall exercise three to four times a day.
Surgical Treatment
Since there are many different causes of flatfoot, the types of flatfoot reconstruction surgery are best categorized by the conditions. Posterior tibial tendon dysfunction. In this condition, the tendon connecting the calf muscle to the inner foot is torn or inflamed. Once the tendon is damaged it no longer can serve its main function of supporting the arch of the foot. Flatfoot is the main result of this type of condition and can be treated by the following flatfoot reconstruction surgeries. Lengthening of the Achilles tendon. Otherwise known as gastrocnemius recession, this procedure is used to lengthen the calf muscles in the leg. This surgery treats flatfoot and prevents it from returning in the future. This procedure is often combined with other surgeries to correct posterior tibial tendon dysfunction. Cleaning the tendon. Also known as tenosynovectomy, this procedure is used in the earlier and less severe stages of posterior tibial tendon dysfunction. It is performed before the arch collapses and while the tendon is only mildly affected. The inflamed tissue is cleaned away and removed from the remaining healthy tendon. Tendon transfer. This procedure is done to correct flatfoot and reform the lost arch in the foot. During the procedure, the diseased tendon is removed and replaced by tendon from another area of the foot. If the tendon is only partially damaged, the inflamed part is cleaned and removed then attached to a new tendon. Cutting and shifting bones. Also called an osteotomy, this procedure consists of cutting and reconstructing bones in the foot to reconstruct the arch. The heel bone and the midfoot are most likely reshaped to achieve this desired result. A bone graft may be used to fuse the bones or to lengthen the outside of the foot. Temporary instrumentation such as screws and plates can also be used to hold the bones together while they heal.
Prevention
Sit up straight in a chair with your feet flat on the ground. Scrunch up the toes of one foot as if you are trying to grab hold of the floor then use your toes to drag your foot a small distance forwards. Do this a couple of times on each foot, but don?t use your leg muscles to push your foot forward -- the movement should come solely from the muscles in your feet. Sit in a chair and place a cleaning cloth, towel or small ball on the floor at your feet. Use the toes of one foot to grasp the object and lift it off the floor. This action will require you to clench your toes and contract your arch. Once you have lifted the object a little way off the floor, try to throw it in the air and catch it by stretching your toes and arch out and upwards. Repeat the exercise several times on both feet. Sit on the floor with your legs straight out in front of you then bend your knees out to either side and place the soles of your feet together so your legs form a diamond. Hold on to your ankles and, keeping your heels together at all times, separate your feet so your toes point out to either side. Open and close your feet in this way several times, making sure your little toes stay in contact with the floor throughout the exercise. Starting in the same position, try separating your heels, keeping your toes together at all times.
Leg Length Discrepancy Surgical Treatment
Overview
Epiphysiodesis is a surgical option designed to slow down the growth of the long leg over a period of months to years. It is only used in growing children. The operation involves a general anaesthetic. Small incisions are made around the knee near the growth plates of the thigh bone and the shin bone. The growth plates are prevented from growing by the use of small screws and plates (?8 - plates?). The screws are buried beneath the skin and are not visible. Stitches are buried beneath the skin and do not need to be removed. The child is normally in hospital for 2-3 days. The child can weight bear immediately and return back to normal activity within a few weeks. Long term follow up is required to monitor the effects of the surgery. The timing of the surgery is based on the amount of growth predicted for the child. Therefore, this procedure can under- and over-correct the difference in leg length. Occasionally the screws have to be removed to allow growth to continue. This procedure can be used on one half of the growth plate to correct deformity in a limb e.g. knock-knees or bow legs. This is known as hemiepiphysiodesis.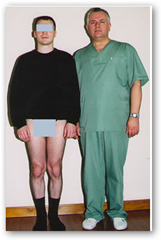
Causes
Leg discrepancy can develop from a medical issue in any portion of the femur or tibia. One leg may lengthen, but leg shortening is much more common. Factors that can cause leg length discrepancy include inherited growth deficiencies. Infections. A bone infection can cause delayed growth in the affected limb. Injury. If your child breaks a leg, it may be shorter once it heals. This is most likely to happen if the fracture or break was complicated, an open fracture, or an injury that affected the growth plate near the end of the bone. Alternatively, a break can cause bones to grow faster after healing, making a leg longer. Tumors. Legg-Calve-Perthes disease. This is a condition that affects the ball (femoral head) of the hip joint. The femoral head may be friable and damage easily, sometimes leading to shortening of the thigh bone. Hemihypertrophy. In children with this condition, one side of the body grows more quickly than the other. Vascular malformations. These are abnormal clusters of veins and arteries that can form close to the bone and stimulate growth. Juvenile arthritis. Inflammation from arthritis can stimulate growth in the affected leg and cause discrepancy.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

leg length discrepancy measurement
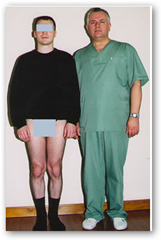
Surgical Treatment
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.
Epiphysiodesis is a surgical option designed to slow down the growth of the long leg over a period of months to years. It is only used in growing children. The operation involves a general anaesthetic. Small incisions are made around the knee near the growth plates of the thigh bone and the shin bone. The growth plates are prevented from growing by the use of small screws and plates (?8 - plates?). The screws are buried beneath the skin and are not visible. Stitches are buried beneath the skin and do not need to be removed. The child is normally in hospital for 2-3 days. The child can weight bear immediately and return back to normal activity within a few weeks. Long term follow up is required to monitor the effects of the surgery. The timing of the surgery is based on the amount of growth predicted for the child. Therefore, this procedure can under- and over-correct the difference in leg length. Occasionally the screws have to be removed to allow growth to continue. This procedure can be used on one half of the growth plate to correct deformity in a limb e.g. knock-knees or bow legs. This is known as hemiepiphysiodesis.
Causes
Leg discrepancy can develop from a medical issue in any portion of the femur or tibia. One leg may lengthen, but leg shortening is much more common. Factors that can cause leg length discrepancy include inherited growth deficiencies. Infections. A bone infection can cause delayed growth in the affected limb. Injury. If your child breaks a leg, it may be shorter once it heals. This is most likely to happen if the fracture or break was complicated, an open fracture, or an injury that affected the growth plate near the end of the bone. Alternatively, a break can cause bones to grow faster after healing, making a leg longer. Tumors. Legg-Calve-Perthes disease. This is a condition that affects the ball (femoral head) of the hip joint. The femoral head may be friable and damage easily, sometimes leading to shortening of the thigh bone. Hemihypertrophy. In children with this condition, one side of the body grows more quickly than the other. Vascular malformations. These are abnormal clusters of veins and arteries that can form close to the bone and stimulate growth. Juvenile arthritis. Inflammation from arthritis can stimulate growth in the affected leg and cause discrepancy.
Symptoms
Faulty feet and ankle structure profoundly affect leg length and pelvic positioning. The most common asymmetrical foot position is the pronated foot. Sensory receptors embedded on the bottom of the foot alert the brain to the slightest weight shift. Since the brain is always trying to maintain pelvic balance, when presented with a long left leg, it attempts to adapt to the altered weight shift by dropping the left medial arch (shortening the long leg) and supinating the right arch to lengthen the short leg.1 Left unchecked, excessive foot pronation will internally rotate the left lower extremity, causing excessive strain to the lateral meniscus and medial collateral knee ligaments. Conversely, excessive supination tends to externally rotate the leg and thigh, creating opposite knee, hip and pelvic distortions.
Diagnosis
Infants, children or adolescents suspected of having a limb-length condition should receive an evaluation at the first sign of difficulty in using their arms or legs. In many cases, signs are subtle and only noticeable in certain situations, such as when buying clothing or playing sports. Proper initial assessments by qualified pediatric orthopedic providers can reduce the likelihood of long-term complications and increase the likelihood that less invasive management will be effective. In most cases, very mild limb length discrepancies require no formal treatment at all.
Non Surgical Treatment
In some circumstances, the physician will recommend a non-surgical form of treatment. Non-surgical treatments include orthotics and prosthetics. Orthotics are a special type of lift placed in or on a shoe that can be used in the treatment of leg length discrepancies between two and six centimeters. In pediatric patients who have large discrepancies and are not good candidates for other treatment forms, prosthetics can be helpful.

leg length discrepancy measurement
Surgical Treatment
Differences of an inch-and-a-half to two inches may require epiphysiodesis (adjusting the growth of the longer side) or acute shortening of the other side. Differences greater than 2.5 inches usually require a lengthening procedure. The short bone is cut and an external device is applied. Gradual lengthening is done over months to allow the muscles and nerves accommodate the new length.
Working with Mortons Neuroma
Overview
 Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Causes
Inappropriate footwear is one of the principle causes of Morton?s neuroma. Toe spring and tapering toe boxes are the most problematic shoe design features that contribute to this health problem. Morton?s neuroma occurs when one of your nerves is stretched and pinched, which happens with great frequency in people who wear shoes incorporating these design features. A professional shoe fitting should always be sought if you are struggling with neuroma-related symptoms.
Symptoms
Patients with a Morton's neuroma typically experience a sharp, shooting or burning pain, usually at the base of the forefoot or toes, which radiates into the two affected toes. Sometimes the pain may also radiate into the foot. The pain is often associated with the presence of pins and needles and numbness.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe, as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Treatment for Morton's neuroma may depend on several factors, including the severity of symptoms and how long they have been present. The earlier on the condition is diagnosed, the less likely surgery is required. Doctors will usually recommend self-help measures first. These may include resting the foot, massaging the foot and affected toes. Using an ice pack on the affected area (skin should not be directly exposed to ice, the ice should be in a container or wrapped in something) Changing footwear, wearing wide-toed shoes, or flat (non high-heeled) shoes. Trying arch supports (orthotic devices). A type of padding that supports the arch of the foot, removing pressure from the nerve. The doctor may recommend a custom-made, individually designed shoe-insert, molded to fit the contours of the patient's foot. There are several OTC (over the counter, non-prescription) metatarsal pads or bars available which can be placed over the neuroma. Taking over-the-counter, non-prescription painkilling medications. Modifying activities, avoiding activities which put repetitive pressure on the neuroma until the condition improves. Bodyweight management,if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with foot problems, such as flat feet, who successfully lose weight experience considerable improvement of symptoms.
Surgical Treatment
Surgery for Morton's neuroma is usually a treatment of last resort. It may be recommended if you have severe pain in your foot or if non-surgical treatments haven't worked. Surgery is usually carried out under local anaesthetic, on an outpatient basis, which means you won't need to stay in hospital overnight. The operation can take up to 30 minutes. The surgeon will make a small incision, either on the top of your foot or on the sole. They may try to increase the space around the nerve (nerve decompression) by removing some of the surrounding tissue, or they may remove the nerve completely (nerve resection). If the nerve is removed, the area between your toes may be permanently numb. After the procedure you'll need to wear a special protective shoe until the affected area has healed sufficiently to wear normal footwear. It can take up to four weeks to make a full recovery. Most people (about 75%) who have surgery to treat Morton's neuroma have positive results and their painful symptoms are relieved.
Prevention
Although the exact causes of neuromas are not completely known, the following preventive steps may help. Make sure your exercise shoes have enough room in the front part of the shoe and that your toes are not excessively compressed. Wear shoes with adequate padding in the ball of the foot. Avoid prolonged time in shoes with a narrow toe box or excessive heel height (greater than two inches).
 Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.
Morton's neuroma is the common name given to the nerve irritation that is found in the ball of the foot that may or may not be accompanied by an inter-metatarsal bursae (a bursa-neuromal complex). It is often associated with inflammation or degeneration and often occurs with constant pressure or irritation of the nerve from the surrounding bony structures or local bursas (fluid filled sacs). Morton's Neuroma can cause symptoms such as a sharp pain, burning even a lack of feeling in the ball of the foot and associated toes.Causes
Inappropriate footwear is one of the principle causes of Morton?s neuroma. Toe spring and tapering toe boxes are the most problematic shoe design features that contribute to this health problem. Morton?s neuroma occurs when one of your nerves is stretched and pinched, which happens with great frequency in people who wear shoes incorporating these design features. A professional shoe fitting should always be sought if you are struggling with neuroma-related symptoms.
Symptoms
Patients with a Morton's neuroma typically experience a sharp, shooting or burning pain, usually at the base of the forefoot or toes, which radiates into the two affected toes. Sometimes the pain may also radiate into the foot. The pain is often associated with the presence of pins and needles and numbness.
Diagnosis
Patients with classic Morton?s neuroma symptoms will have pain with pressure at the base of the involved toes (either between the 2nd and 3rd toes, or between the 3rd and 4th toes). In addition, squeezing the front of the foot together can exacerbate symptoms. As well, they may have numbness on the sides of one toe and the adjacent toe, as this corresponds with the distribution of the involved nerve.
Non Surgical Treatment
Treatment for Morton's neuroma may depend on several factors, including the severity of symptoms and how long they have been present. The earlier on the condition is diagnosed, the less likely surgery is required. Doctors will usually recommend self-help measures first. These may include resting the foot, massaging the foot and affected toes. Using an ice pack on the affected area (skin should not be directly exposed to ice, the ice should be in a container or wrapped in something) Changing footwear, wearing wide-toed shoes, or flat (non high-heeled) shoes. Trying arch supports (orthotic devices). A type of padding that supports the arch of the foot, removing pressure from the nerve. The doctor may recommend a custom-made, individually designed shoe-insert, molded to fit the contours of the patient's foot. There are several OTC (over the counter, non-prescription) metatarsal pads or bars available which can be placed over the neuroma. Taking over-the-counter, non-prescription painkilling medications. Modifying activities, avoiding activities which put repetitive pressure on the neuroma until the condition improves. Bodyweight management,if the patient is obese the doctor may advise him/her to lose weight. A significant number of obese patients with foot problems, such as flat feet, who successfully lose weight experience considerable improvement of symptoms.

Surgical Treatment
Surgery for Morton's neuroma is usually a treatment of last resort. It may be recommended if you have severe pain in your foot or if non-surgical treatments haven't worked. Surgery is usually carried out under local anaesthetic, on an outpatient basis, which means you won't need to stay in hospital overnight. The operation can take up to 30 minutes. The surgeon will make a small incision, either on the top of your foot or on the sole. They may try to increase the space around the nerve (nerve decompression) by removing some of the surrounding tissue, or they may remove the nerve completely (nerve resection). If the nerve is removed, the area between your toes may be permanently numb. After the procedure you'll need to wear a special protective shoe until the affected area has healed sufficiently to wear normal footwear. It can take up to four weeks to make a full recovery. Most people (about 75%) who have surgery to treat Morton's neuroma have positive results and their painful symptoms are relieved.
Prevention
Although the exact causes of neuromas are not completely known, the following preventive steps may help. Make sure your exercise shoes have enough room in the front part of the shoe and that your toes are not excessively compressed. Wear shoes with adequate padding in the ball of the foot. Avoid prolonged time in shoes with a narrow toe box or excessive heel height (greater than two inches).
How Shoe Lifts Cure Leg Length Imbalances
There are not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is anatomically shorter than the other. Through developmental phases of aging, the brain senses the stride pattern and identifies some variance. The human body typically adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch isn't grossly irregular, require Shoe Lifts to compensate and typically doesn't have a profound effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, however this issue is very easily remedied, and can eliminate many incidents of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts . These are generally very reasonably priced, in most cases being less than twenty dollars, compared to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Mid back pain is the most widespread health problem affecting men and women today. Around 80 million people are affected by back pain at some stage in their life. It is a problem that costs businesses huge amounts of money annually on account of time lost and production. Innovative and better treatment methods are constantly sought after in the hope of lowering economical influence this condition causes.

People from all corners of the earth suffer from foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of very beneficial. The lifts are capable of reducing any discomfort and pain in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists.
To be able to support the human body in a balanced fashion, the feet have a critical job to play. In spite of that, it can be the most overlooked area of the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This causes other parts of the body including knees, ankles and backs to be affected too. Shoe Lifts make sure that correct posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, however this issue is very easily remedied, and can eliminate many incidents of upper back pain.
Therapy for leg length inequality commonly consists of Shoe Lifts . These are generally very reasonably priced, in most cases being less than twenty dollars, compared to a custom orthotic of $200 or more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Mid back pain is the most widespread health problem affecting men and women today. Around 80 million people are affected by back pain at some stage in their life. It is a problem that costs businesses huge amounts of money annually on account of time lost and production. Innovative and better treatment methods are constantly sought after in the hope of lowering economical influence this condition causes.

People from all corners of the earth suffer from foot ache as a result of leg length discrepancy. In these situations Shoe Lifts might be of very beneficial. The lifts are capable of reducing any discomfort and pain in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists.
To be able to support the human body in a balanced fashion, the feet have a critical job to play. In spite of that, it can be the most overlooked area of the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This causes other parts of the body including knees, ankles and backs to be affected too. Shoe Lifts make sure that correct posture and balance are restored.
What Is A Inferior Calcaneal Spur

Overview
Heel spurs, or abnormal growths of the heel bone, can cause sharp pains in the heel, especially first thing in the morning and after long periods of rest. In many cases, a heel spur develops as a result of plantar fasciitis, which is the inflammation of the ligament that stretches along the bottom of the foot, from the base of the toes to the heel. In individuals who suffer from plantar fasciitis, the ligament pulls away from the heel as the foot bears weight. In an effort to stabilize the ligament, the body may produce calcium deposits, which can then develop into heel spurs.
Causes
Heel spurs can form as a result of repeated strain placed on foot muscles and ligaments as well as from abnormally stretching the band of tissue connecting the heel and ball of the foot. Repeated injury to the membrane that lines the heel bone can also cause problems as can repeated tight pressure on the back of the heel. The causes can range from excessive walking (especially if unaccustomed to walking), running or jumping to improperly fitted or worn-out shoes. Runners, volleyball players, and tennis players, people who do step aerobics or stair climbing for exercise, those with flat feet, pregnant women, the obese and diabetics and those who wear tight-fitting shoes with a high heel are all prone to developing spurs (and plantar fasciitis) more readily.

Symptoms
If your body has created calcium build-ups in an effort to support your plantar fascia ligament, each time you step down with your foot, the heel spur is being driven into the soft, fatty tissue which lines the bottom of your heel. Heel spur sufferers experience stabbing sensations because the hard protrusion is literally being jabbed into the heel pad. If left untreated, Plantar Fasciitis and heel spurs can erode the fatty pad of the heel and cause permanent damage to the foot. Fortunately, most cases can be resolved without medications or surgeries.
Diagnosis
The proper diagnosis of a heel spur often requires an X-ray. To make this process as convenient for his patients as possible, most clinics have an on-site digital X-ray and diagnostic ultrasound machines. This can make it unnecessary for patients to visit diagnostic imaging centers, allowing patients to receive more expedient treatment.
Non Surgical Treatment
Heel spurs are considered a self-limited condition, which means that by making small alterations in your lifestyle and regular routines you can often control the condition. The goal is to relieve pain, reduce friction and transfer pressure from your sensitive foot areas. By eliminating the cause of the heel spur and plantar fasciitis (i.e. better shoes, orthotics to fix your gait, losing weight) will help reduce the pressure put on your fascia and heel and can reduce the inflammation caused by your heel spur. Failure to see improvements after conservative treatments may make surgery your only option.
Surgical Treatment
Usually, heel spurs are curable with conservative treatment. If not, heel spurs are curable with surgery, although there is the possibility of them growing back. About 10% of those who continue to see a physician for plantar fascitis have it for more than a year. If there is limited success after approximately one year of conservative treatment, patients are often advised to have surgery.
Prevention
There are heel spur prevention methods available in order to prevent the formation of a heel spur. First, proper footwear is imperative. Old shoes or those that do not fit properly fail to absorb pressure and provide the necessary support. Shoes should provide ample cushioning through the heel and the ball of the foot, while also supporting the arch. Wearing an orthotic shoe insert is one of the best ways to stretch the plantar fascia and prevent conditions such as heel spurs. Stretching the foot and calf is also helpful in preventing damage. Athletes in particular should make sure to stretch prior to any physical activity. Stretching helps prevent heel spurs by making tissue stronger as well as more flexible. In addition, easing into a new or increasingly difficult routine should be done to help avoid strain on the heel and surrounding tissue.
What Is A Posterior Calcaneal Spur

Overview
Bone spurs are bony projections that develop along the edges of bones. Bone spurs (osteophytes) often form where bones meet each other - in your joints. They can also form on the bones of your spine. The main cause of bone spurs is the joint damage associated with osteoarthritis. Most bone spurs cause no symptoms and may go undetected for years. They may not require treatment. Decisions about treatment depend on where spurs are situated and how they affect your health.
Causes
When the Plantar Fascia is allowed to rest during sleep or long periods of inactivity, the fascia tightens and shortens. When you first stand up after resting, the fascia is forced to stretch very quickly causing micro-tears in the tissue. This is why the first steps in the morning are so exquisitely painful. Heel spurs are more likely to happen if you suffer from over-pronation (walking with a rolling gait) you stand or walk on rigid surfaces for long periods, you are above ideal weight or during pregnancy, you have stiff muscles in your calves.

Symptoms
Major symptoms consist of pain in the region surrounding the spur, which typically increases in intensity after prolonged periods of rest. Patients may report heel pain to be more severe when waking up in the morning. Patients may not be able to bear weight on the afflicted heel comfortably. Running, walking, or lifting heavy weight may exacerbate the issue.
Diagnosis
Because the diagnosis of heel spurs can be confused with tarsal tunnel syndrome (as described earlier), most surgeons advocate performing a tarsal tunnel release (or at least a partial tarsal tunnel release) along with the plantar fascia release. This surgery is about 80percent successful in relieving pain in the small group of patients who do not improve with conservative treatments.
Non Surgical Treatment
Treatment of heel spurs is the same as treatment of plantar fasciitis. Because these problems are related, the treatment is the same. The first step in the treatment of a heel spur is short-term rest and inflammation control. Here are the steps patients should take in order to cure the symptoms of plantar fasciitis and heel spurs. Avoiding the activity that caused the symptoms is the first step in treatment. For example, take a few day off jogging or prolonged standing/walking. Just resting usually helps to eliminate the most severe pain, and will allow the inflammation to begin to cool down. Icing will help to diminish some of the symptoms and control the heel pain. Icing is especially helpful after a sudden flare up of symptoms. Exercises and stretches are designed to relax the tissues that surround the heel bone. Some simple exercises, performed in the morning and evening, often help patients feel better quickly. Many patients will work with a physical therapist, or you can try some simple activities on your own. If you need some help, meet with a therapist for a few sessions to learn a program you can continue on your own.
Surgical Treatment
In some cases, heel spurs are removed by surgery after an X-ray. While the surgery is typically effective, it?s a timely and expensive procedure. Even after surgery, heel spurs can re-form if the patient continues the lifestyle that led to the problem. These reasons are why most people who develop painful heel spurs begin looking for natural remedies for joint and bone pain. Surgery isn?t required to cure a heel spur. In fact, more than 90 percent of people get better with nonsurgical treatments. If nonsurgical methods fail to treat symptoms of heel spurs after 12 months, surgery may be necessary to alleviate pain and restore mobility.
Prevention
You can help prevent heel spur symptoms from returning by wearing the proper shoes. Customized orthotics and insoles can help relieve pressure. It is important to perform your exercises to help keep your foot stretched and relaxed.
Bursa Foot Surgery Recuperation
Overview
Swelling and inflammation near a joint may be a sign of bursitis, a condition that involves buildup of liquid and inflammation in a bursa sac that cushions a joint. This condition has earned some interesting names over the years: housemaid?s knee, student?s elbow, and tailor?s bottom, to name a few. Simply put, bursitis is the inflammation of a bursa and buildup of fluid in the bursa sac. A bursa is a thin, slippery sac found around a joint that serves to reduce friction between bone and surrounding soft tissue, such as skin, muscles, ligaments and tendons. A bursa sac is made up of a synovial membrane, or synovium, that produces and contains synovial fluid. Excessive friction, a trauma, or other condition can irritate the synovium and cause it to become inflamed. The inflamed synovium will thicken and produce excess synovial fluid, and can cause symptoms such as localized swelling, skin redness and warmth, tenderness and pain. Of the approximately 160 bursae in the body, only a handful of them usually cause bursitis. These usual suspects are found in the knee, shoulder, elbow, and hip. Less frequently, bursitis may also occur in the heel, wrist, buttocks and big toe.
Causes
A bursa acts as a cushion and lubricant between tendons or muscles sliding over bone. There are bursas around most large joints in the body, including the ankle. The retrocalcaneal bursa is located in the back of the ankle by the heel. It is where the large Achilles tendon connects the calf muscles to the heel bone. Repeated or too much use of the ankle can cause this bursa to become irritated and inflamed. Possible causes are too much walking, running, or jumping. This condition is usually linked to Achilles tendinitis. Sometimes retrocalcaneal bursitis may be mistaken for Achilles tendinitis. Risks for this condition include starting an aggressive workout schedule, or suddenly increasing activity level without the right conditioning.
Symptoms
Limping. Decreased movement. Your ankles may feel stiff or unable to move as well as they usually do. Pain or tenderness in the back of the ankle. It may be worse at the beginning of exercise, or when running uphill. You may also have pain when wearing shoes. Redness and warmth. If the bursa is infected, the skin over the heel may be red and warm. You may also have a fever. Swelling on the back of the heel.
Diagnosis
A thorough subjective and objective examination from a physiotherapist may be all that is necessary to diagnose a retrocalcaneal bursitis. Diagnosis may be confirmed with an ultrasound investigation, MRI or CT scan.
Non Surgical Treatment
Your health care provider may recommend the following treatments. Avoid activities that cause pain. Ice the heel several times a day. Take nonsteroidal anti-inflammatory medications (for example, ibuprofen). Try over-the-counter or custom heel wedges to help decrease the stress on the heel. Try ultrasound treatment during physical therapy to reduce inflammation. Use physical therapy to improve flexibility and strength around the ankle, which can help the bursitis improve and prevent it from coming back. If these treatments don't work, your health care provider may inject a small amount of steroids into the bursa. After the injection, you should avoid stretching the tendon too much because it can break open (rupture). If the condition is connected with Achilles tendinitis, casting the ankle for several weeks to keep it from moving can be effective. Very rarely, surgery may be needed to remove the inflamed bursa.
Surgical Treatment
Only if non-surgical attempts at treatment fail, will it make sense to consider surgery. Surgery for retrocalcanel bursitis can include many different procedures. Some of these include removal of the bursa, removing any excess bone at the back of the heel (calcaneal exostectomy), and occasionally detachment and re-attachment of the Achilles tendon. If the foot structure and shape of the heel bone is a primary cause of the bursitis, surgery to re-align the heel bone (calcaneal osteotomy) may be considered. Regardless of which exact surgery is planned, the goal is always to decrease pain and correct the deformity. The idea is to get you back to the activities that you really enjoy. Your foot and ankle surgeon will determine the exact surgical procedure that is most likely to correct the problem in your case. But if you have to have surgery, you can work together to develop a plan that will help assure success.
Prevention
Once your pain and inflammation is gone, you can prevent retrocalcaneal bursitis deformity by wearing the best shoes for your foot type. You should high-heels and pumps if possible. Wear orthotics (custom arch supports) or over-the-counter orthotic devices. Perform frequent Achilles tendon stretching exercises to prevent it from becoming tight agian. Avoiding running uphill when training. Try to run on softer surfaces and avoid concrete.
Swelling and inflammation near a joint may be a sign of bursitis, a condition that involves buildup of liquid and inflammation in a bursa sac that cushions a joint. This condition has earned some interesting names over the years: housemaid?s knee, student?s elbow, and tailor?s bottom, to name a few. Simply put, bursitis is the inflammation of a bursa and buildup of fluid in the bursa sac. A bursa is a thin, slippery sac found around a joint that serves to reduce friction between bone and surrounding soft tissue, such as skin, muscles, ligaments and tendons. A bursa sac is made up of a synovial membrane, or synovium, that produces and contains synovial fluid. Excessive friction, a trauma, or other condition can irritate the synovium and cause it to become inflamed. The inflamed synovium will thicken and produce excess synovial fluid, and can cause symptoms such as localized swelling, skin redness and warmth, tenderness and pain. Of the approximately 160 bursae in the body, only a handful of them usually cause bursitis. These usual suspects are found in the knee, shoulder, elbow, and hip. Less frequently, bursitis may also occur in the heel, wrist, buttocks and big toe.
Causes
A bursa acts as a cushion and lubricant between tendons or muscles sliding over bone. There are bursas around most large joints in the body, including the ankle. The retrocalcaneal bursa is located in the back of the ankle by the heel. It is where the large Achilles tendon connects the calf muscles to the heel bone. Repeated or too much use of the ankle can cause this bursa to become irritated and inflamed. Possible causes are too much walking, running, or jumping. This condition is usually linked to Achilles tendinitis. Sometimes retrocalcaneal bursitis may be mistaken for Achilles tendinitis. Risks for this condition include starting an aggressive workout schedule, or suddenly increasing activity level without the right conditioning.
Symptoms
Limping. Decreased movement. Your ankles may feel stiff or unable to move as well as they usually do. Pain or tenderness in the back of the ankle. It may be worse at the beginning of exercise, or when running uphill. You may also have pain when wearing shoes. Redness and warmth. If the bursa is infected, the skin over the heel may be red and warm. You may also have a fever. Swelling on the back of the heel.
Diagnosis
A thorough subjective and objective examination from a physiotherapist may be all that is necessary to diagnose a retrocalcaneal bursitis. Diagnosis may be confirmed with an ultrasound investigation, MRI or CT scan.
Non Surgical Treatment
Your health care provider may recommend the following treatments. Avoid activities that cause pain. Ice the heel several times a day. Take nonsteroidal anti-inflammatory medications (for example, ibuprofen). Try over-the-counter or custom heel wedges to help decrease the stress on the heel. Try ultrasound treatment during physical therapy to reduce inflammation. Use physical therapy to improve flexibility and strength around the ankle, which can help the bursitis improve and prevent it from coming back. If these treatments don't work, your health care provider may inject a small amount of steroids into the bursa. After the injection, you should avoid stretching the tendon too much because it can break open (rupture). If the condition is connected with Achilles tendinitis, casting the ankle for several weeks to keep it from moving can be effective. Very rarely, surgery may be needed to remove the inflamed bursa.
Surgical Treatment
Only if non-surgical attempts at treatment fail, will it make sense to consider surgery. Surgery for retrocalcanel bursitis can include many different procedures. Some of these include removal of the bursa, removing any excess bone at the back of the heel (calcaneal exostectomy), and occasionally detachment and re-attachment of the Achilles tendon. If the foot structure and shape of the heel bone is a primary cause of the bursitis, surgery to re-align the heel bone (calcaneal osteotomy) may be considered. Regardless of which exact surgery is planned, the goal is always to decrease pain and correct the deformity. The idea is to get you back to the activities that you really enjoy. Your foot and ankle surgeon will determine the exact surgical procedure that is most likely to correct the problem in your case. But if you have to have surgery, you can work together to develop a plan that will help assure success.
Prevention
Once your pain and inflammation is gone, you can prevent retrocalcaneal bursitis deformity by wearing the best shoes for your foot type. You should high-heels and pumps if possible. Wear orthotics (custom arch supports) or over-the-counter orthotic devices. Perform frequent Achilles tendon stretching exercises to prevent it from becoming tight agian. Avoiding running uphill when training. Try to run on softer surfaces and avoid concrete.